If you’re little one is experiencing reactions to foods after introduction of solids, I am so sorry. I know the real fear and anxiety you’re likely feeling as a parent, but rest assured you’re in the right place. This article covers the topic of Baby Allergy Testing highlighting two common allergenic foods, peanuts and cow’s milk, for babies. It covers not only what the science says, but also a registered dietitian mother’s firsthand experience going through the food allergy testing process with her 6 and a half month old baby boy.

If you’ve landed on this page, I’m truly sending you the biggest warm hug. I know as a parent how nerve wrecking infant food allergies are. But, rest assured, you’re in good hands because I’m about to walk you through the available science wearing my dietitian hat while showing your first hand as a mother how this process went for my son.
If you’re tight on time, use this table of contents to select the portion of this post you’d like to jump too. Sending you lot’s of patience and grace as you go through this journey.
Jump to:
What is a Food Allergy
A food allergy is when an individual has an immune response after eating a specific food.
While there are considered now 9 allergenic foods, sesame, the newest addition, soy, wheat, eggs, milk, peanuts, treenuts, fish, and shellfish, there are a few that seem to be more allergenic for babies.
The top allergens that infants usually react to include:
- Peanuts
- Milk (cow’s)
- Egg
- Treenuts
- Soy
Now, the type of immune system’s response can have a wide range of symptoms, from mild to severe.
Mild symptoms of a food allergy reaction can include:
- Itching, skin rashes and hives, swelling of the lips, face, tongue, wheezing, congestion, nausea, vomiting, and/or diarrhea.
More severe symptoms that involve anaphylaxis, a life-threatening condition, include:
- Construction of the airways, difficulty breathing, increased heart-rate, low blood pressure, and/or dizziness or light headedness.
While these symptoms aren’t exhaustive and can be more intense in one individual over another, they are common when it comes to food allergies and important to pay attention too.
Risk Factors for Infant Food Allergies
Research shows that there are three situations in particular that can actually increase the potential for an infant developing a food allergy
Skin Conditions: Eczema or Dermatitis
While having a skin condition like eczema or dermatitis doesn’t automatically mean your child will have a food allergy, research does show kids with these conditions are more likely to have a food allergy. Approximately 27% of children with food allergy had reported eczema or skin allergy, compared with 8% of children without food allergy.
Family History of Siblings with Food Allergies
Research shows that infants who have a sibling with a food allergy may be at a higher risk for developing a food allergy. According to the results of this study, 13.6% of infants born to a family with a sibling that has a food allergy also were clinically reactive to a food.
These results found that milk allergy was the most common allergy among siblings (5.9%), followed by egg allergy (4.4%) and peanut allergy (3.7%).
Gender and Ethnicity
Research has found food allergies tend to be higher in children, non-Hispanic blacks, and males.
Indications for Testing a Baby For Food Allergies
If you’re child has any of the risk factors listed above coupled with any signs or symptoms of experiencing an allergic reaction after consuming foods, then it’s a good idea to speak with your pediatrician about food allergy testing.
In my personal experience, my son, other than being male, had no risk factors setting him at higher risk for developing a food allergy.
However, after introducing him to solids at around 5 months with no signs or symptoms of an allergy developing, he began to break out in hives. It was approximately 4 weeks into his solid journey that we noticed the below rash develop after he ate Greek yogurt (made from cow’s milk) and peanuts.

This reaction occurred twice over the weekend and thankfully we were already scheduled for his 6-month appointment early Monday morning, so I took these photos into the doctor to see what she recommended we do.
The below photo is another skin reaction he experienced after his sister, my three year old toddler, had a cow’s milk smoothie then kissed him.
While both of these reactions were baffling to me, especially after he had tolerated both foods for over a month with at least a dozen introductions without problems, I’ve quickly learned that the dosing and frequency with allergenic foods is very important, even when your child may not necessarily be at higher risk for developing a food allergy.
Don’t worry if you’re a little confused here as well, I’ll dive into this a bit more below.
How Allergy Testing in Babies is Done
After you consult with your pediatrician, they will more often than not send you to an allergist trained in pediatrics to begin the evaluation period.
There are a few different options for testing for food allergies, including the skin prick test, a blood test, an oral food challenge test, and an elimination diet.
The skin prick test (SPT) and blood test help identify if your body has an immune mediated reaction to the protein found in a specific food and an antibody known as Ig-E (immunoglobulin-E).
However, just because your child may experience a reaction to the skin prick test when exposed to the potentially allergenic food or tests positive for the Ig-E antibody in their blood, this does not necessarily mean they have a food allergy. Skin prick tests and blood tests both experience a 50-60% false positive result. Let’s jump into now what each different test looks like.
Skin Prick Testing
The skin prick test involves using a small amount of the suspected allergenic food (or environmental allergen) and applying that to the skin to evaluate how the body responds to its presence. The SPT is minimally invasive (it’s sort of like a small fingernail scratch on the skin), inexpensive, and yields immediate results.
Depending on your allergist protocol, they will often have a control known as a histamine placed at the top of the back to use as a benchmark for the other suspects under question.
The photo below of my son when he underwent his first skin prick test with the 8 foods he had been exposed to over the weekend when he had his first reaction (which included the cow’s milk and peanut allergens.)

After the allergenic food is applied, the patient needs to still still for 15 minutes before results can be read to evaluate the Ig-E reaction.
Parents who are trying to get this test done solo while having your baby sit still, you deserve a giant latte after this!
Having gone through this myself for my own environmental allergies and experiencing the constant itching I felt in the course of that time span I was very worried with how my son would respond.
While it wasn’t easy keeping him still in a tiny 6×6-ft mini room, we prevailed by bouncing him on my knee to prevent his back from rubbing against anything and playing with the stroller ball covered in ribbons. I highly encourage you to have a toy or something attached to your stroller that you can use for entertainment during this test!
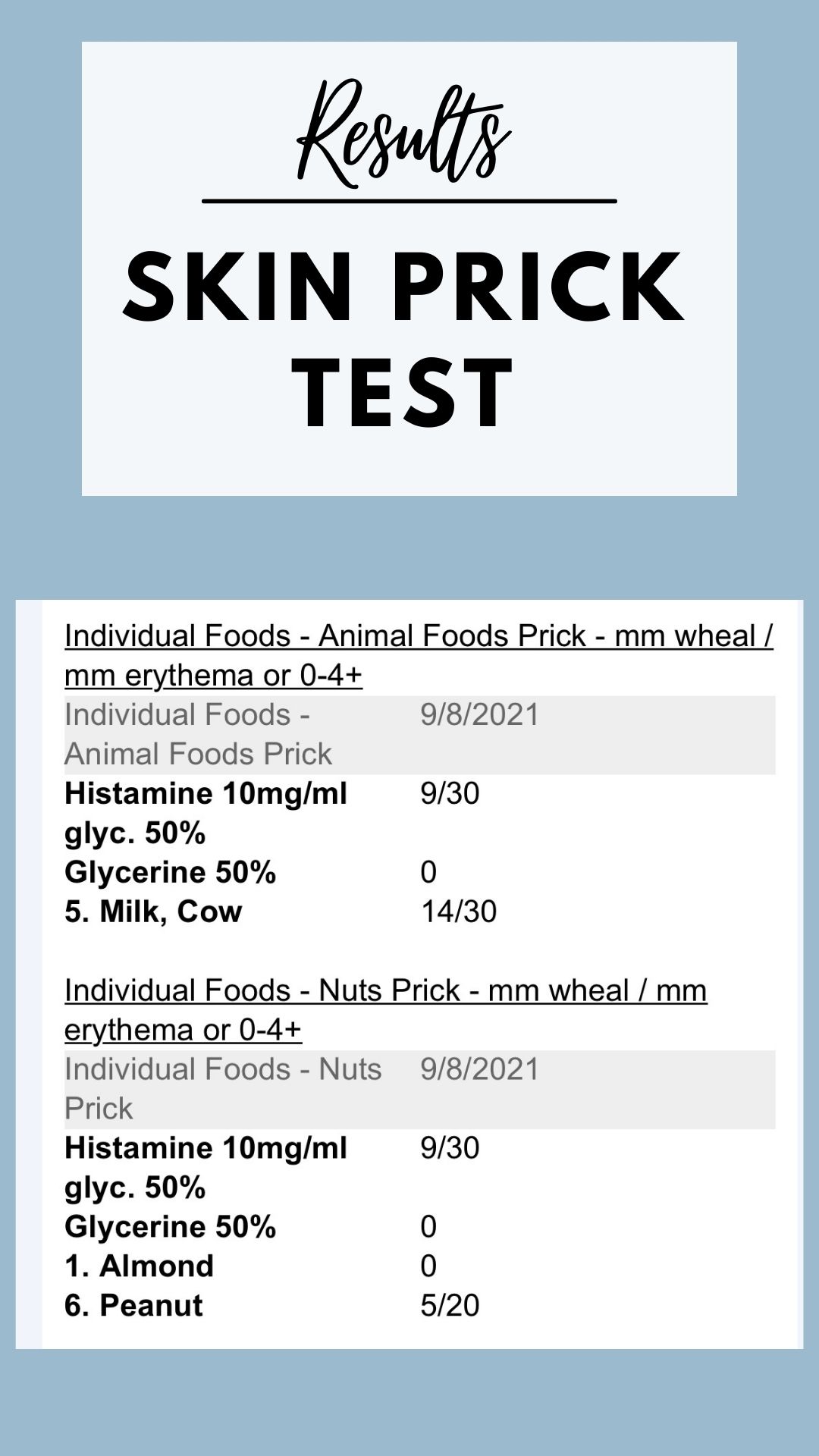
Our Results: SPT
The results of the SPT are immediate as I mentioned. When you leave your doctors office, not only will you visibly be able to see what your child reacted too, but you will have access to test results like these.
Blood Test for IG-E Antibodies
The blood test for food allergies is “simply” a blood test that takes a few days to get results. I say “simply” in a sarcastic tone, because while this is a standard blood draw for an adult, for an infant, it’s very traumatic (or maybe more for the mom, TBD.)
Nonetheless, you have to pin your infant down while the phlebotomist takes two tubes of blood for testing. Given my track record of rolling veins, my son too had his “disappear” which resulted in the lab tech having to prick him in each arm and “dig around” with the needle until they finally located a vein to get the blood out of.
While the photo below is clearly before this experience happened, I will say he did sleep very well after this (likely due to the trauma of it for us all!)
Results: Blood Test
It took approximately 6 business days to get the results (included below) for the blood test to identify which foods he also was experiencing the Ig-E antibody production too. Since there are a few different options available for the blood tests, it’s best to discuss them with your doctor (as with anything) before consulting Dr. Google!
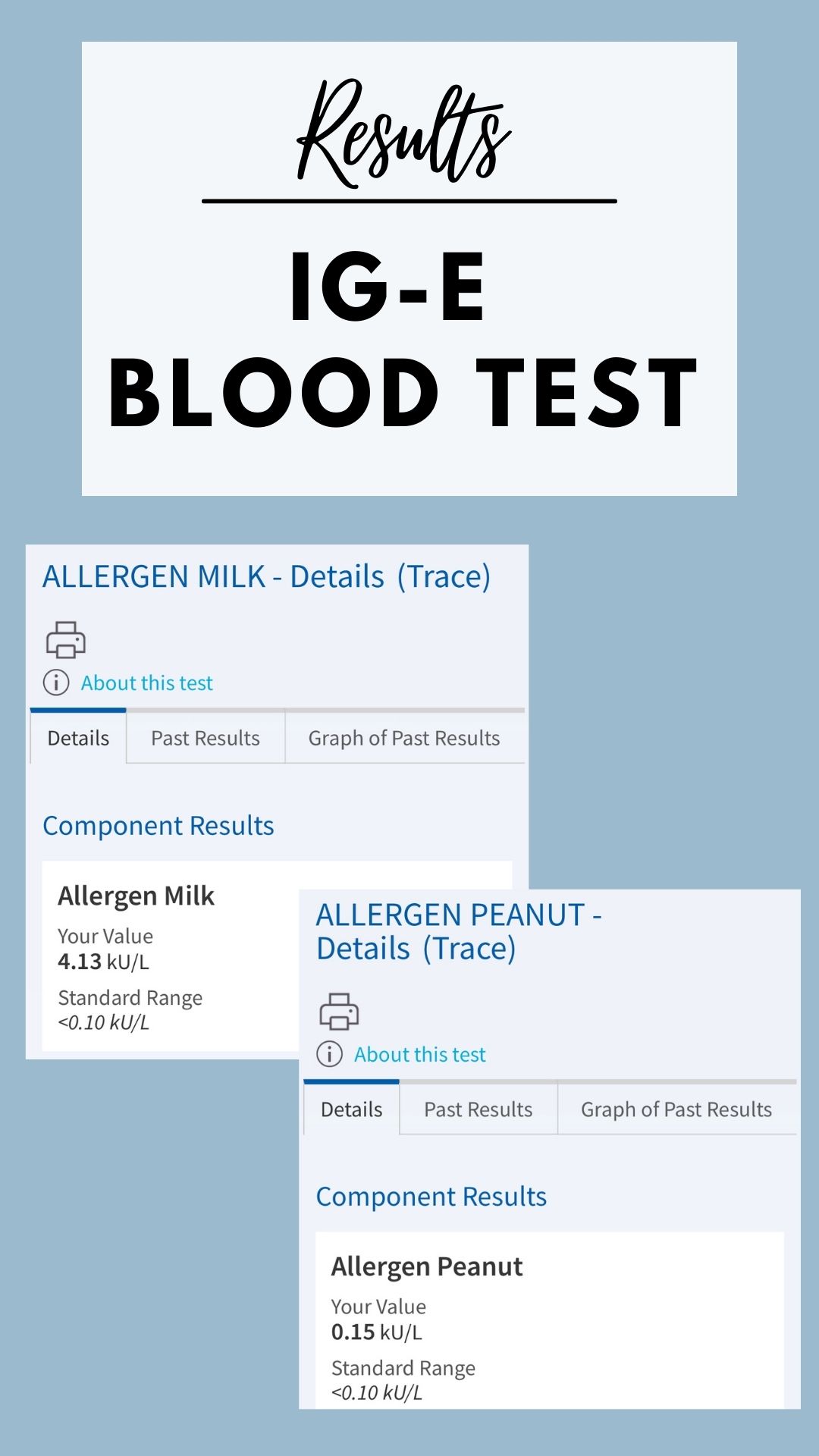
It’s important to note that while these results indicated my son was allergic to both peanuts and milk, the higher result for the milk in comparison to the peanut does not necessarily mean he is “more severely” allergic to milk.
Rather, this just means he is in fact experiencing an Ig-E mediated reaction that should warrant a discussion about scheduling an OFC.
False-Positive Food Allergy Results – What This Means
As I mentioned above, there is a 50-60% change that the SPT and blood test can yield a positive result when in fact the individual is not allergic to that food. This usually occurs for two reasons:
- The individual’s digestive system acts on breaking down the protein enough from the food that it is no longer consider a threat and thus the body does not react to it.
- The individual is allergic to a similar food in the same family but the true allergenic food has yet to be identified. For instance, if the test indicates an allergy to cashews but you child is able to tolerate them, they may be allergic another tree nut in the family, such as almonds.
Depending on the results and the professional opinion of your allergist, they will typically move forward with recommending proceeding with another test option.
Oral Food Challenge Test
The oral food challenge (OFC) test is the most time intensive of all tests. Under the supervision of your allergist, your child will receive increasing doses of an allergenic food while be closely monitored for signs and symptoms.
You will be given specific instructions on the type of food to bring for testing depending on the allergen they are going to be evaluating. Some facilities will even have a specific recipe you will need to prepare to bring in for baked egg or milk challenges.

After your child consumes the food in increasing increments (usually 15 to 20 minutes) over an hour, the medical team will evaluate them for any signs or symptoms of an allergic reaction. If they experience anything significant, you medical team will be there to provide assistance and stop the test if needed.
Depending on the allergenic food, the OFC is used to help figure out if a a level of “safe exposure” can be offered at home to help the child outgrow a food allergy.
A standard OFC will generally yield accurate results, but the symptoms can also be delayed. For this reason, the OFC regulations require patients stay at least 2-3 hours minimum after the last food is tested to monitor for reactions.
For a deeper dive into the OFC research, I recommend taking a look at this 2019 study.
Results of OFC
While the method and record keeping may differ slightly amongst providers, here is a sample of both the peanut and baked milk OFC’s my son underwent.
Peanut OFC
For this challenge, we brought in powdered peanut butter and an unsweetened applesauce and breastmilk to serve it with. This was very easily tolerated with my 6.5 month old and easy to serve him. If I had brought in Bamba, the peanut puff snack, he would have had to eat 21 sticks to receive the level of protein exposure to perform the test which would have been very challenging for his age and size.
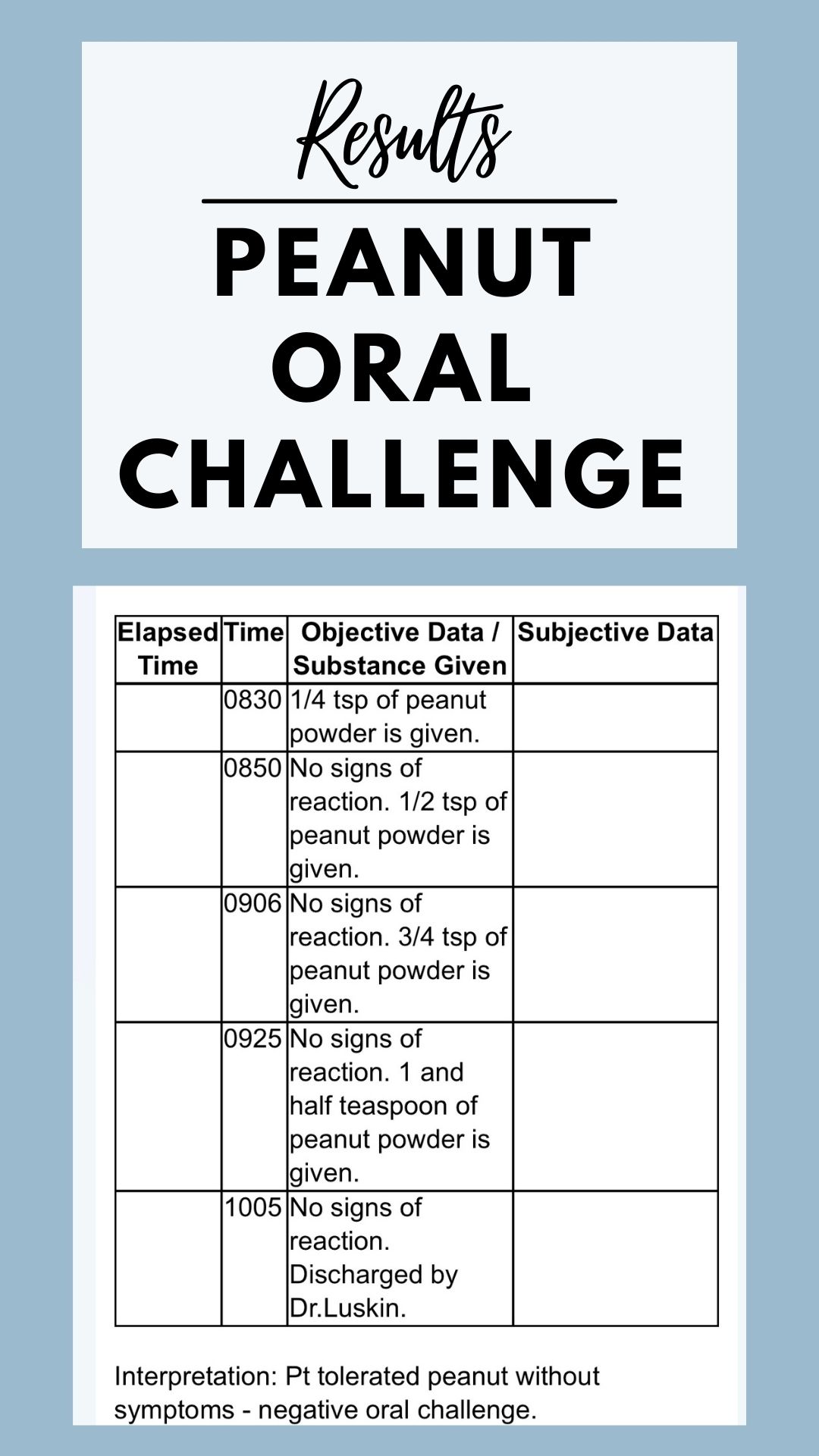
While my son did not react in the doctors office to the peanut powder, he has since reacted with a few mild rashes at home upon giving him other forms of peanuts. We are discussing now with our doctor how to proceed, but it appears to only be topical and non-irritating.
Though this is alarming as a parent, I do want to continue with the safe level of oral food protein exposure at home so we can hopefully fully outgrow his reactions one day. We do have an epipen now and are in communication with our allergist to ensure we continue to do exposure safely.
Baked Milk OFC
For this challenge, we modified the facility preferred baked milk muffin recipe we were given by swapping out the added sugar since technically babies under 2 years of age should not be given added sugar.
I used about 70% less of a date sugar in the recipe to provide a small amount of sweetness, and then brought with me breastmilk to soften the muffin with so he could actually eat it with a spoon in a more appropriate texture for his age.
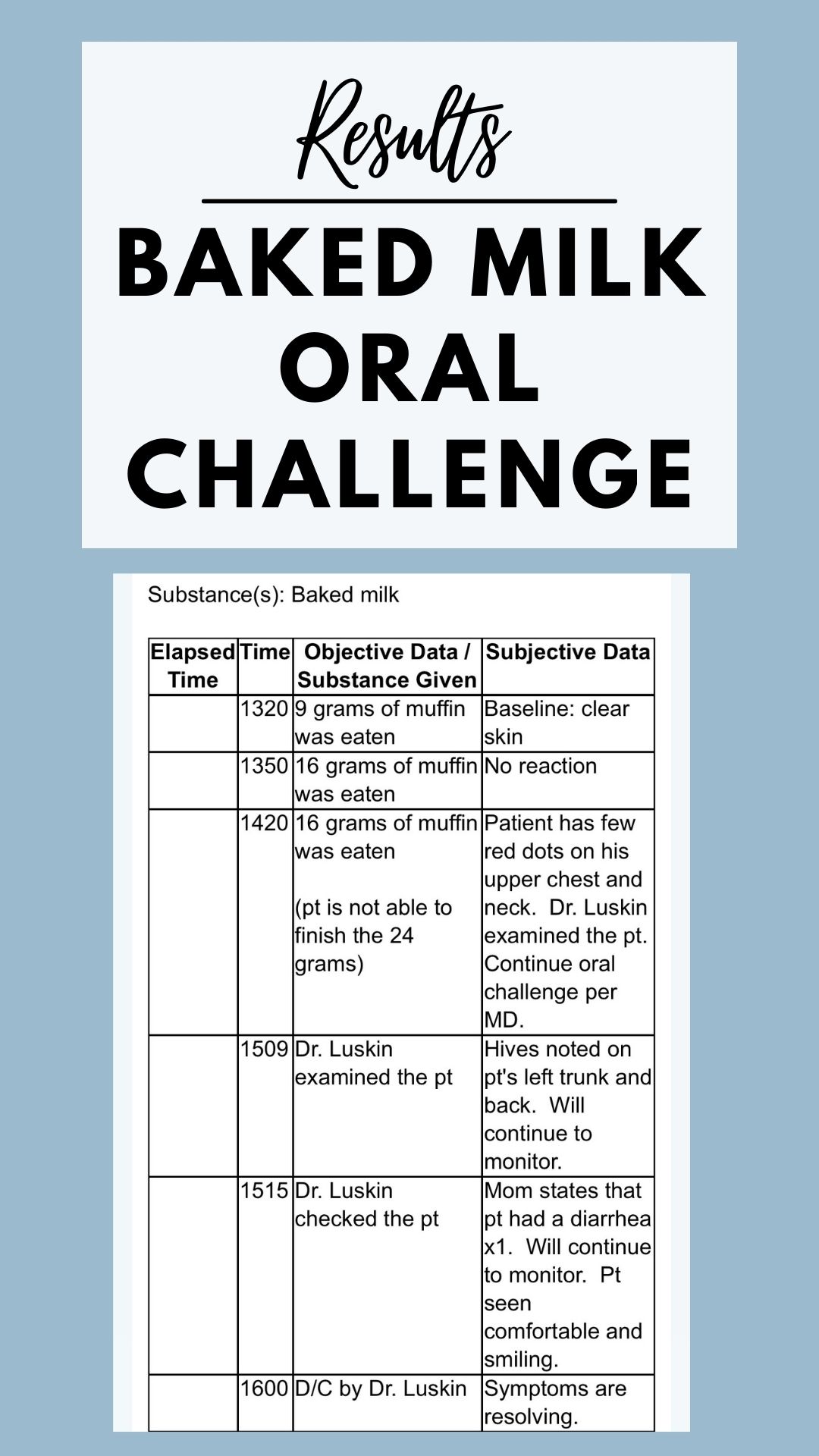
About an hour or so after my son had three exposures to the muffin, he began to develop hives on his body and then had a bout of diarrhea. This was indicative he has a confirmed allergic reaction to cow’s milk.
For now, we are refraining from offering any form of cow’s milk, baked or in it’s natural state, in his diet. Since he is breastfed, I have also modified my own diet to refrain from dairy at this time due to the allergists recommendations. Though my son was not in pain nor experiencing any diarrhea or hives after nursing when I was still eating cow’s milk dairy items, I did notice the amount of vomit after his feeds goes down when I do not have dairy in my diet. This is still not confirmed if it was the dairy in my diet, or my strong letdown reflux.
Nothing can be that black-and-white I’m finding when it comes to your kids, right?!
Now, there may be ways to safely incorporate milk into a nursing mothers’ diet through working with a trained dietitian in food allergies. The research is continually evolving on the intersection of what amount is passed from mother to baby through breastmilk, but of course there are multiple factors at play that effect this (i.e. genetics, digestion, etc.)
You should always consult with your child’s allergist and follow their recommendations.
Elimination Diets
An elimination diet is just what it sounds like! You would eliminate the food in question for 2 to 4 weeks under the guidance of your doctor (and hopefully dietitian!)
While elimination diets offer an opportunity to see if a particular food is causing the symptoms your child is experiencing, professionally I do not find that these sorts of diets work well with the younger population as far as truly understanding the food(s) causing the reaction.
This is largely in part of that fact that if the reaction is in the gut and causing symptoms that the person would need to communicate (i.e. an upset stomach, pain, etc.) the infant or small child may not be able to.
Personally, this is also not something I’d want to pursue with my infant until I knew for certain the results of some of the other forms of testing mentioned above because I would want to ensure I knew for certain if the reaction was Ig-E mediated and the true response to consumption of the food. This data would help one understand if they needed to have an epipen prescription.
As always, discuss with your child’s team the best plan for their particular situation.
Understanding Pediatric Food Allergy Prevention Recommendations
Current recommendations are vastly different from what our parents likely were taught when most of us started solids (i.e. refrain from introducing the top food allergens to infants until they are at least one year of age).
Instead, the recent studies that indicate early introduction is powerful in helping to prevent food allergy development.
It’s important to work with your pediatrician if your child has any of the risk factors mentioned above when introducing the top food allergens in their diet.
If your child (like mine) does not have any of the risk factors placing them at a higher risk for a food allergy, it’s important to follow the research recommendations that suggest introducing foods, like peanuts and egg, early and often can help prevent the development of a food allergy later in life.
There is a wonderful website, BabysFirst.org, produced by the Food Allergy Research and Education Organization (FARE) that helps parents with starting solids with the allergenic foods.
Solid Food Introduction Recommendations
For peanuts specifically, there is research that shows introducing peanuts at least 3 times a week in 2 gram doses (about 1.5 teaspoons of peanut powder or 21 Bamba) can reduce the risk of your child developing a peanut food allergy.
While there are no specific amounts for the other allergenic foods, it’s important to remember continual, gradual exposure is key.
However, remember, this is for low risk infants. Consider the following tips regardless of your child’s risk factor as you explore introducing the 9 top allergenic foods into their diets.
Tips to Remember with Food Allergen Solids Introduction
- Serve at home where you can be present and aware of your child’s response.
- Only offer one new food at once until you can monitor their response. Then you can offer combination foods after you’ve ruled out an allergen.
- Monitor your child closely.
- Start small and slow, gradually increasing dosage to meet recommendations.
Where to Get More Information on Pediatric Food Allergies
- Sign up for the Food Allergy Research and Education newsletter and consult their website! It’s filled with wonderful information.
- If you’re a healthcare professional, consider watching this great webinar, “Food Allergy vs Food Intolerance”, by a fellow RDN!
- Consider working with a dietitian trained in food allergies. Three wonderful colleagues I have are Sherry Coleman Collins, The Lifestyle Dietitian, and Healthy Mom Healthy Kids!
Thanks so much for stopping by! If you enjoyed this post, please consider sharing it with a friend and tagging me on social: Facebook, Instagram, or Pinterest.



Leave a Reply